RHINOPLASTY
Rhinoplasty, also referred to as nose surgery or nasal reshaping, is a procedure that alters the structure of the nose. It may be performed for functional reasons (such as improving breathing) or cosmetic purposes (to adjust the size or shape of the nose).
This surgery is tailored to each individual and may involve changes to the nasal bones, cartilage, skin, or all three. Your surgeon will assess your specific anatomy and discuss your goals to determine the most appropriate approach.
Also Known As:
- Nose reshaping
- Nasal surgery
- Functional rhinoplasty
- Cosmetic rhinoplasty
- Septo-rhinoplasty (when combined with septal correction)
Rhinoplasty Techniques
There are various rhinoplasty techniques used depending on the individual's nasal structure, goals, and functional concerns. The approach may involve open or closed techniques and can focus on changes to the bone, cartilage, or soft tissue. In some cases, the procedure may be combined with septoplasty to address both form and function.
During your consultation, your surgeon will conduct a detailed assessment of your nasal anatomy and overall facial features to help determine the most appropriate surgical approach.
Who May Consider Rhinoplasty?
Rhinoplasty may be appropriate for individuals who:
- Wish to change the size, shape, or profile of their nose
- Experience breathing difficulties due to internal nasal structure
- Have experienced trauma or injury affecting nasal function or symmetry
- Have reached facial maturity and are in good overall health
- Have realistic expectations regarding the outcome of surgery
Common Rhinoplasty Techniques
- Open Rhinoplasty: Ideal for intricate cases, offering enhanced visibility of underlying structures with a small external incision on the columella.
- Closed Rhinoplasty: Suitable for less complex cases, with all incisions inside the nostrils and no visible external scars.
- Augmentation Rhinoplasty: For increasing nose size using cartilage grafts or synthetic implants.
- Reduction Rhinoplasty: Ideal for those with larger noses, this technique reduces size for better facial symmetry.
- Functional Rhinoplasty: Focused on correcting breathing issues like a deviated septum or nasal valve collapse.
What to Expect During Rhinoplasty Surgery
Rhinoplasty is a tailored surgical procedure that involves detailed planning and technique selection based on your anatomy and individual goals. The following steps outline what may be involved in the procedure:
- Pre-operative Consultation. A comprehensive consultation is conducted to discuss your medical history, examine nasal structure, and clarify expectations. This includes an evaluation of both aesthetic and functional concerns.
- Digital Imaging (Optional). In some cases, digital simulations may be used to help communicate potential outcomes. It's important to note that these images are for illustrative purposes only and results may vary.
- Anaesthesia. Rhinoplasty is usually performed under general anaesthesia. Your surgeon will discuss the type of anaesthesia used and any associated considerations prior to surgery.
- Incision Technique. Two primary techniques may be used:
- Open Rhinoplasty: An incision is made across the columella (the tissue between the nostrils) for greater access to the nasal structures.
- Closed Rhinoplasty: Incisions are made inside the nostrils, with no external scar.
The choice of technique depends on the complexity of the procedure and the areas being addressed.
- Reshaping the Nose. The underlying nasal structure—bone and cartilage—may be altered through trimming, repositioning, or grafting, depending on the surgical goals.
- Septoplasty (if required). If functional issues such as breathing difficulties are present, procedures like septoplasty may be performed to correct a deviated septum and improve nasal airflow.
- Tip Modification. The nasal tip can be refined by adjusting the underlying cartilage to improve proportion and alignment with the rest of the nose and face.
- Bridge Adjustments. Humps or depressions on the nasal bridge may be smoothed or filled to improve overall structure.
- Closure and Initial Support. Incisions are closed with fine sutures. Internal or external splints may be applied to support the nose and aid in maintaining shape during the early healing period.
Rhinoplasty Recovery
Recovery following rhinoplasty varies between individuals and depends on the complexity of the procedure and the patient’s general health. Below is a general guide to what you may expect during the post-operative period:
Immediate Post-Operative Period
- After surgery, patients are typically monitored in a recovery area for a short time before being discharged on the same day.
- You will need a responsible adult to accompany you home and remain with you for the first 24 hours.
First Week
- Most patients are advised to rest at home during the initial week and avoid any strenuous activity.
- Prescribed medications, including pain relief and antibiotics (if needed), should be taken as directed.
- Sleeping with your head elevated can help minimise swelling.
Swelling and Bruising
- Swelling and bruising around the eyes and nose are common and usually peak within the first 48–72 hours.
- Cold compresses may help reduce swelling in the early days following surgery.
- While swelling gradually decreases, some residual swelling may persist for several months.
Nasal Splints and Dressings
- Nasal splints or dressings may be applied to support the nose during initial healing.
- These are typically removed during a follow-up appointment within the first 7–14 days.
Returning to Daily Activities
- Many individuals return to work or light duties after one to two weeks, depending on comfort and recovery progress.
- Activities that increase blood pressure or risk nasal injury (e.g. intense exercise, contact sports) should be avoided for several weeks, or until cleared by your surgeon.
Long-Term Recovery
- Subtle changes in nasal shape and internal structure can continue to evolve for up to 12–18 months post-surgery.
- Functional improvements (e.g. breathing) may also gradually become more noticeable over time.
- Ongoing follow-up with your surgeon is important to assess healing and outcomes.
Potential Risks – Rhinoplasty
Rhinoplasty is a surgical procedure to reshape or refine the structure of the nose. It may be performed for cosmetic, functional, or reconstructive reasons. As with any surgery, rhinoplasty carries general and procedure-specific risks that should be carefully considered:
- Infection at the surgical site, which may require antibiotics or further treatment
- Bleeding or haematoma, which may require medical attention
- Scarring, particularly if an open rhinoplasty technique is used (scars are typically minimal and placed discreetly at the base of the nose)
- Breathing difficulties, especially if internal structures are altered or swelling obstructs the nasal passages
- Septal perforation (a hole in the nasal septum), which is uncommon but may cause breathing issues, crusting, or whistling
- Altered sense of smell, usually temporary but may be prolonged in rare cases
- Skin numbness or changes in sensation around the nose or upper lip, usually temporary
- Persistent swelling, particularly at the nasal tip, which can take many months to fully resolve
- Poor wound healing or delayed recovery, more common in smokers or individuals with certain medical conditions
- Anaesthesia-related risks, including allergic reactions or complications related to sedation or general anaesthesia
If you have any questions or wish to discuss Rhinoplasty options, please contact our clinic to schedule a consultation with Dr Reema Hadi.
If you would like more information on Rhinoplasty, you can visit the Australian Society of Plastic Surgery
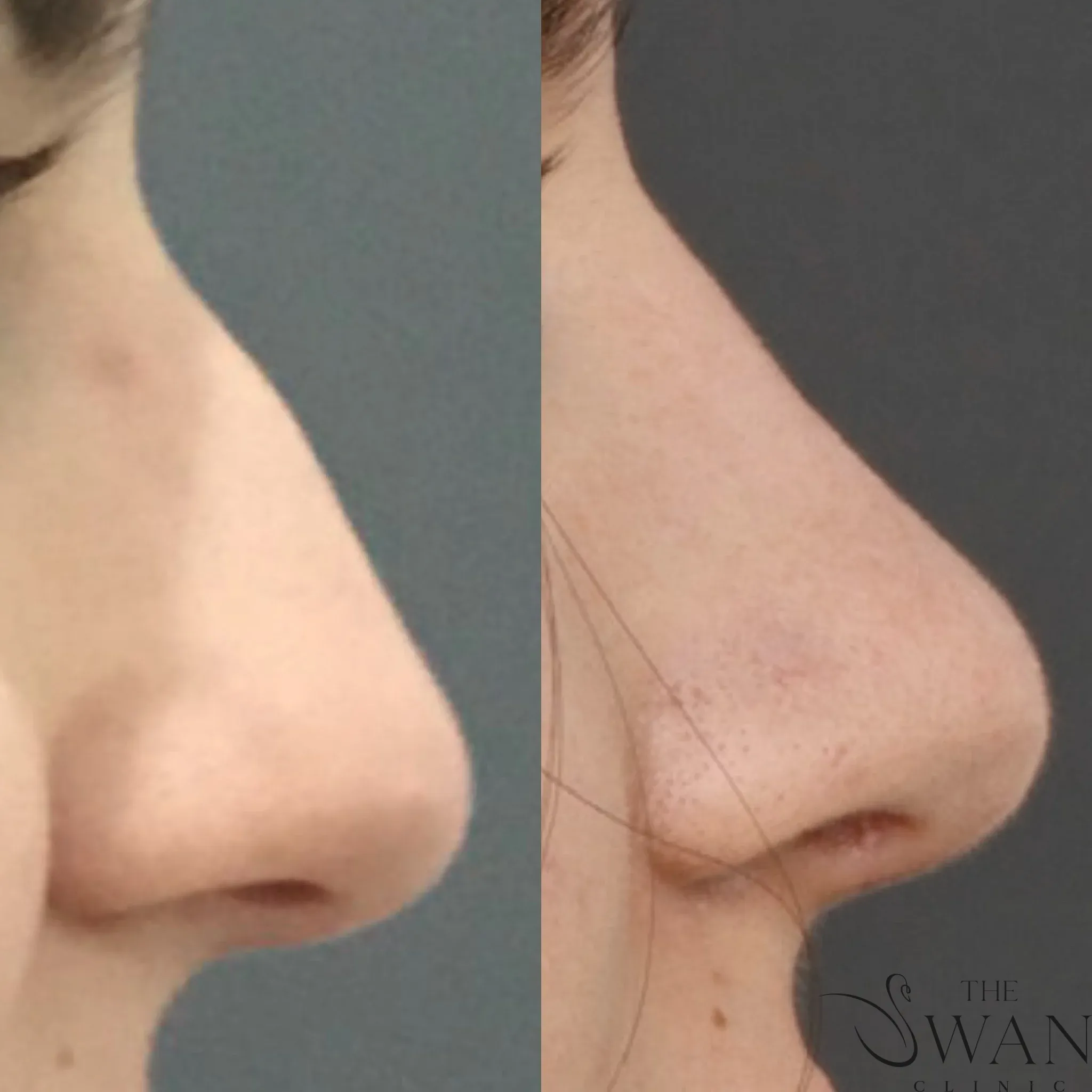
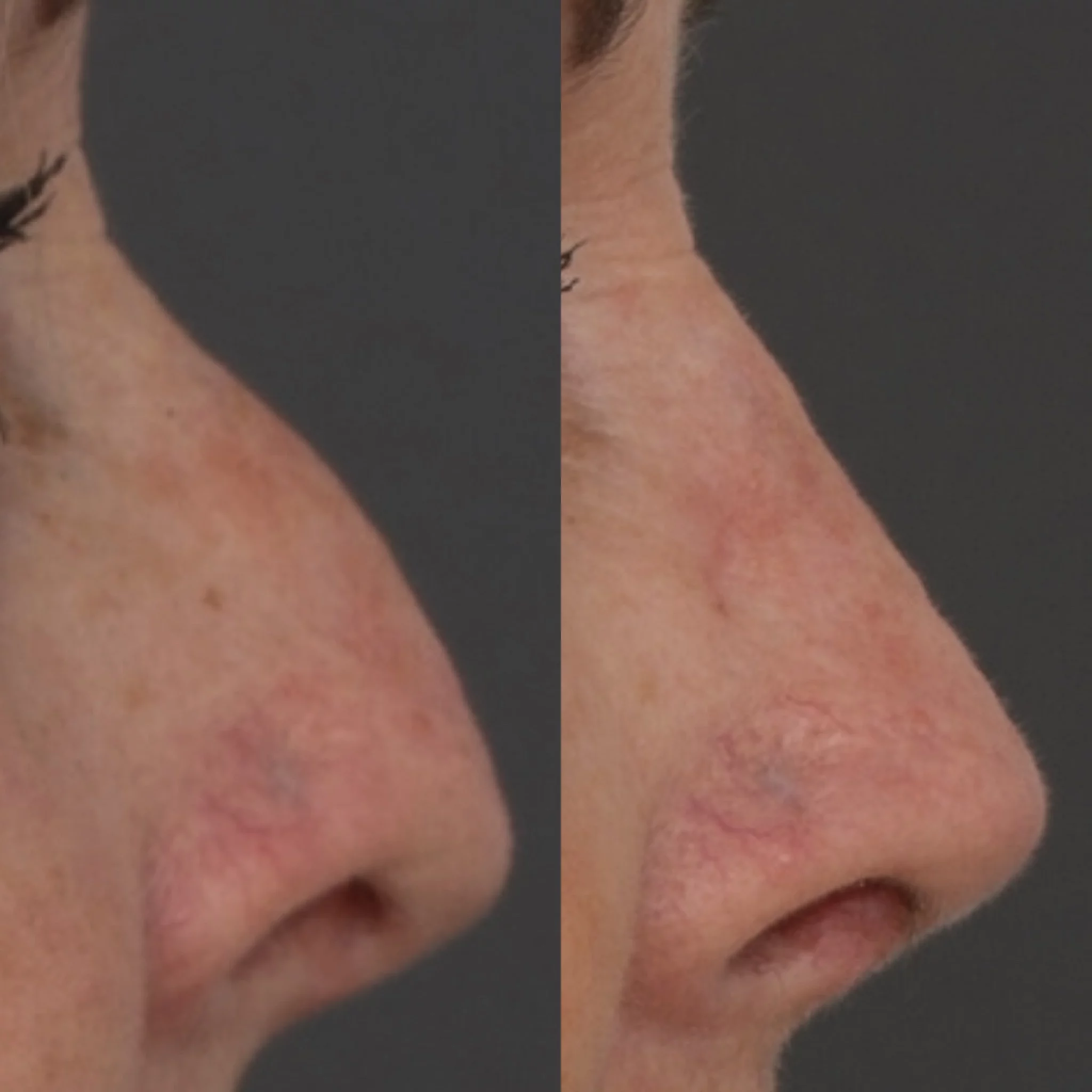
Before and After Photos
Real patient results from our expert procedures